In the trial, for the first time, clinical researchers will attempt to correct a harmful beta-globin gene mutation in a patient's own cells with non-virally delivered CRISPR gene-correction tools, according to Mark Walters, MD, a professor of pediatrics at UCSF and principal investigator of the clinical trial and gene editing project.
"This therapy has the potential to transform sickle cell disease care by producing an accessible, curative treatment that is safer than the current therapy of stem cell transplant from a healthy bone marrow donor," Walters said. "If successfully applied in young patients, it has the potential to prevent irreversible complications of the disease."
Sickle cell disease is a genetic blood disorder that affects the structure and function of hemoglobin, reduces the ability of red blood cells to transport oxygen efficiently, and progresses to a chronic vascular disease that affects approximately 100,000 Americans and millions worldwide, with a disproportionate effect on the Black community.
The CRISPR-Cas9 clinical trial furthers BCH Oakland's commitment to treating and finding a cure for sickle cell disease. The Comprehensive Sickle Cell Disease Center was created at the hospital in 1973 to provide expert diagnosis, treatment and long-term health management for children and adults with sickle cell disease. Now known as the BCH Oakland Sickle Cell Center of Excellence, the center is recognized as having one of the largest and most comprehensive sickle cell programs in the Western United States.
The trial will combine CRISPR technology developed at Innovative Genomics Institute (IGI) (a joint UC Berkeley-UCSF initiative founded by Nobel Laureate Jennifer Doudna); UCLA's expertise in genetic analysis and cell manufacturing, as well as its clinical excellence in the field; and nearly 50 years of expertise at BCH Oakland in sickle cell care, including cord blood and marrow transplantation, and gene therapy.
"The use of CRISPR gene editing to fix the mutation causing sickle cell disease in each patient's own blood-forming stem cells required the development of new methods to produce more than 100 million cells per patient that are gene-corrected, healthy and pure," said Donald Kohn, MD, medical director of the UCLA Human Gene and Cell Therapy Facility. "Previous research studies were limited to producing ½ to 2 million genetically corrected cells, so this represents a significant increase in scale."
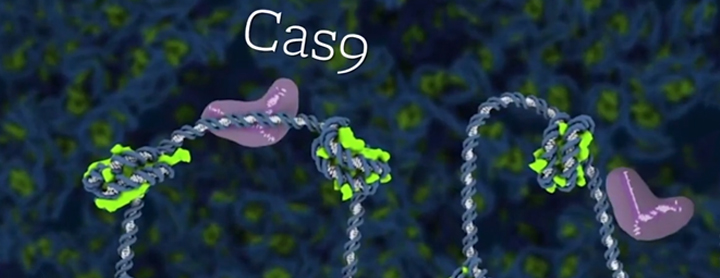
The disease is caused by a single-letter change, or mutation, in human DNA. This trial will use CRISPR genome editing to correct that mutation directly. The project team from UCSF, the IGI and UCLA have developed CRISPR_SCD001, a patient-specific blood stem cell therapy that has been modified by a CRISPR-Cas9 nuclease to stimulate repair of the sickle mutation. In the current trial, the patient's blood stem cells will be extracted and sent to UCLA's gene manufacturing lab to be processed, using electrical pulses that create temporary pores in the cell membranes. These pores allow the CRISPR-Cas9 platform to enter the cells and travel to the nucleus, where it corrects the sickle cell mutation before the cells are reintroduced to the patient.
"The goal is to develop a cure that is not just safe and effective, but also affordable to those who need it most," Doudna said. "There have been a lot of promising developments in recent years with CRISPR-based therapies for sickle cell and other genetic diseases, but it's essential to have studies like this that can help us create truly accessible cures."
As part of its legacy, BCH Oakland was recognized for establishing the first not-for-profit sibling donor cord blood bank, leading to children being cured of sickle cell disease and other blood diseases. Among its many accomplishments in treating sickle cell disease, BCH Oakland studied and received FDA approval for the drug voxelotor to improve hemoglobin levels and reduce anemia and hemolysis in sickle cell patients.
As testing of the new CRISPR treatment expands, the UCSF research team is hoping to explore additional resources under development in the UCSF Living Therapeutics Initiative, including the potential to manufacture the investigational cell therapy product at UCSF.